Female reproductive system problems
Reproductive system problems can develop after some types of cancer treatment. Sometimes they happen as a late effect of treatments for cancer during childhood.
The female reproductive system
When a girl is born, her ovaries contain all the eggs they will ever have. When puberty begins, the pituitary gland in the brain signals the ovaries by releasing follicle-stimulating hormone (FSH) and luteinizing hormone (LH). The ovaries then begin to make and release the female hormones estrogen and progesterone, which are necessary for reproductive function.
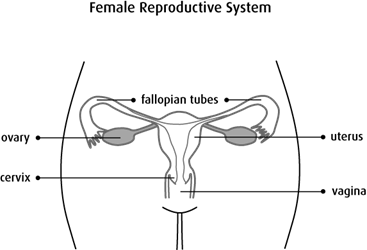
During the normal monthly menstrual cycle, one egg matures and is released from an ovary. This is called ovulation. The lining of the uterus (womb) also grows and thickens. If the egg is not fertilized, the body sheds the lining of the uterus through the vagina. This is called menstruation. The cycle then repeats itself about every 28 days.
With each menstrual cycle, a woman’s supply of eggs lessens. When most of the eggs are gone, menopause begins. During menopause, the menstrual cycles stop, the ovaries stop making hormones and the woman can no longer become pregnant.
Causes
Treatments for cancer, including some types of chemotherapy, radiation therapy and surgery, can cause reproductive system damage for girls and women.
Chemotherapy
Chemotherapy with certain drugs, particularly alkylating drugs, can affect the ovaries. Damage to the ovaries can lead to early, late or absent puberty. It can also lead to early menopause or infertility. Chemotherapy is more likely to damage the ovaries of women who are close to natural menopause, and the damage is more likely to be permanent.
Damage to the reproductive organs is often related to the type and dose of chemotherapy drugs given and the length of treatment. The higher the total dose of chemotherapy, the greater the risk that the ovaries will be damaged.
Chemotherapy used in combination with radiation therapy also increases the risk of damage to the ovaries.
High doses of chemotherapy used in preparation for a stem cell transplant can cause lack of estrogen and infertility.
Chemotherapy drugs that can increase the risk of female reproductive problems include:
- busulfan (Busulfex)
- chlorambucil (Leukeran)
- cisplatin
- cyclophosphamide (Procytox)
- mechlorethamine (nitrogen mustard, Mustargen)
- procarbazine hydrochloride (Matulane)
- lomustine (CeeNU, CCNU)
- carmustine (BiCNU, BCNU)
- melphalan (Alkeran)
- doxorubicin (Adriamycin)
Radiation therapy
The total dose of radiation, area of the body being treated and age at the time of treatment can increase the risk of damage to the reproductive system.
Primary (direct) ovarian failure can happen after radiation to the abdomen, pelvis, lower spine or total body (called total body irradiation, or TBI). Younger girls usually seem to have less damage to the ovaries than girls who are teenagers or young adults during treatment. But higher doses of radiation usually cause the ovaries to stop working in girls and women of all ages.
Secondary (indirect) ovarian failure can happen after radiation therapy to the head. The pituitary gland, which is located in the centre of the brain, controls the production of hormones needed for proper ovarian function. Radiation to the brain at higher doses can damage the pituitary gland, which can lead to low levels of these hormones.
Damage to the uterus can happen after radiation therapy to the pelvis or abdomen. The radiation can damage the muscle of the uterus or the blood vessels that would supply blood to a growing fetus.
Surgery
Surgery for cancers of the reproductive system and for other cancers in the pelvis can cause reproductive problems.
- Surgery to remove the uterus or both ovaries will cause you to be infertile (you won’t be able to get pregnant).
- Surgery in the pelvis can cause scarring that can damage the reproductive organs.
Other factors
Other factors, such as hormonal therapy and some types of targeted immunotherapy drugs, may increase the risk of reproductive problems by causing damage to the ovaries.
Types of female reproductive system problems
Reproductive problems that can develop after treatment for cancer include:
Early, delayed or absent puberty
Puberty usually happens when a girl is 8 to 13 years old. The first signs of puberty are usually the growth of breast buds and hair under the arms and in the pubic area.
Some cancer treatments can affect when puberty starts. It can start earlier (called precocious puberty) or later (called delayed puberty) than normal. Sometimes puberty doesn’t start at all, which is called absent puberty.
Early menopause
Most women go through natural menopause after the age of 40. The average age is 51.
Treatment for cancer can cause the ovaries to stop working and producing estrogen. If this happens before the age of 40, it is called early menopause. Sometimes the ovaries start working again. In other cases, the ovaries don’t start working again and menopause is permanent.
Infertility
Infertility is the inability to become pregnant. It can happen when cancer treatments damage the eggs, uterus, fallopian tubes or ovaries. Sometimes menstrual periods and fertility return after treatment. Other times damage to the reproductive organs is permanent and fertility doesn’t return. Woman closer to the natural age of menopause are at a greater risk of infertility.
Pregnancy problems
Some cancer treatments used during childhood can damage the uterus. This damage can cause problems during pregnancy when the woman is older. The uterus may become less elastic and may be smaller than normal. This can cause a higher risk for a miscarriage or giving birth early (premature delivery). Growth of the fetus in the uterus can also be affected.
Lack of estrogen
When the ovaries are damaged from cancer treatment and don’t make enough estrogen, other problems can develop. Estrogen is needed for reproduction. It’s also important for keeping your bones strong and your heart healthy.
Symptoms
Sometimes cancer treatment damages the ovaries so they can’t release eggs or make hormones. This is called ovarian failure. Symptoms of reproductive system problems related to ovarian failure include:
- no signs of puberty, such as the growth of breast buds and hair under the arms and in the pubic area
- irregular or skipped periods
- premature menopause
- hot flashes or night sweats
- lowered libido (sexual desire)
- vaginal dryness
- fertility problems
- irritability or difficulty concentrating
If symptoms get worse or don’t go away, report them to your doctor or healthcare team without waiting for your next scheduled appointment.
Diagnosis
Your doctor will try to find the cause of your reproductive system problems. You will be asked questions about your symptoms and may have a physical exam. When young girls are treated for cancer, the healthcare team will watch for signs of reproductive problems. They will pay attention to when puberty starts and how it progresses.
You may have blood tests to check the levels of follicle-stimulating hormone, luteinizing hormone and estrogen.
Preventing reproductive system problems
Before a girl or woman starts cancer treatments, fertility counselling may be offered. The fertility counsellor or healthcare team will discuss the possible side effects of treatments that may affect fertility. There are some ways to preserve fertility, but all options may not be available at all healthcare centres.
Egg freezing removes eggs from the ovary and freezes them. Later, they are thawed and fertilized with sperm to form embryos. The embryo is placed in the woman’s uterus when she is ready to get pregnant.
Embryo freezing removes eggs from the ovary, fertilizes them with sperm to form embryos and freezes the embryos for future use.
Radiation shielding is usually done when radiation is given to the abdomen or pelvis, unless the shielding will increase the chance that the cancer will come back. Shields are placed over one or both ovaries and other parts of the reproductive system to help reduce the risk of damage during radiation treatment.
Ovarian transposition( also called oophoropexy) is surgery to move the ovaries to another area of the body to help protect them from the radiation treatment. It may be done during surgery to remove the cancer. After treatment is complete, the ovaries are moved back to their original place.
Managing reproductive system problems
If the healthcare team finds any reproductive system problems after treatment for cancer, you may be referred to one or more of the following specialists:
- an endocrinologist (hormone specialist)
- a gynecologist (specialist in the female reproductive organs)
- a fertility specialist
The healthcare team can suggest ways to manage the following reproductive system problems.
Delayed puberty
Hormonal replacement therapy is given to girls who don’t start puberty. It is used to treat symptoms related to the loss of sex hormone production, such as lack of breast development and loss of normal menstruation.
Early menopause
Symptoms of menopause may be managed with hormone replacement therapy. Young women who want to have children in the future should try to plan pregnancies based on their risk of early menopause.
Talk to your doctor about the risks and benefits of hormone replacement therapy.
Infertility
In vitro fertilization with a donor egg may be an option for women who are infertile. In this procedure, a donor egg (an egg given by someone else) is fertilized with a man’s sperm in a lab. The fertilized egg is then placed in the woman’s uterus.
Pregnancy problems
Studies have shown that most cancer survivors who become pregnant are no more likely to have problems with pregnancy than other women. But some treatments can increase some risks.
Certain chemotherapy drugs, such as anthracyclines, can increase the risk of heart problems during pregnancy, labour and delivery.
Radiation therapy to the uterus can cause poor blood supply to the uterus. This can increase the risk of miscarriage, stillbirth, small babies, low birth weight and premature labour.
Women who have a higher risk for pregnancy problems should be followed closely by an obstetrician who is qualified to care for women with high-risk pregnancies.
Life after treatment
Some women who have had cancer treatment may think that they can’t have children. Because of this belief, they might not use birth control and then have an unplanned pregnancy. Talk to your doctor about your fertility and if you need to use birth control.
Talk to your doctor if you and your partner are considering pregnancy after cancer treatments are over. Your doctor may recommend that you wait at least a 6 months after cancer treatment before trying to conceive. Some doctors may suggest delaying pregnancy for about 2 years after treatment. How long you have to wait depends on many factors, including:
- the type and stage of your cancer
- your prognosis
- your age
- what you prefer or want
Find out more about fertility problems.
Follow-up
All women who are treated for cancer need regular follow-up. The healthcare team will develop a follow-up plan based on the type of cancer, how it was treated and your needs.
Make sure you tell your doctor all the treatments you received. Women who are at risk for reproductive system problems should have a physical exam each year.
During follow-up, your doctor may:
- ask questions about puberty, your menstrual cycle, if you’ve been pregnant and if you’ve had any sexual problems
- do blood tests for levels of follicle-stimulating hormone, luteinizing hormone and estrogen
- do a bone density test to check for osteoporosis
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
