Surgery for stomach cancer
Surgery is often used to treat stomach cancer. The type of surgery you have depends mainly on the size of the tumour and stage of the cancer. When planning surgery, your healthcare team will also consider other factors, such as:
- the type of stomach cancer
- your age
- how well your organs are working and your overall health
- your nutritional status (how well your body's nutritional needs are being met)
Surgery may be done for different reasons. You may have surgery to:
- completely remove the tumour and nearby lymph nodes
- remove as much of the tumour as possible before other treatments
-
rebuild (reconstruct) the
gastrointestinal (GI) tract after the stomach has been removed - ease pain and other symptoms of advanced stomach cancer (called palliative surgery)
The following types of surgery are used to treat stomach cancer. You may also have other treatments before or after surgery.
Surgery for stomach cancer is done using a general anesthetic (a drug that puts you into a deep sleep so you don't feel pain).
Endoscopic resection (ER)
An endoscopic resection (ER) is a specialized surgery used to treat small (smaller than 2 cm), early stage stomach cancer that has not spread beyond the inner lining of the stomach (called the mucosa) or the surrounding connective tissue layer (called the submucosa). The cancer is at a low risk of spreading to nearby lymph nodes.
Depending on how the tissue is removed, an ER can be called an endoscopic mucosal resection (EMR) or an endoscopic submucosal dissection (ESD). An EMR is the more common.
For an ER, an
In Canada, very few stomach cancers are treated with an ER because stomach cancer is rarely found at such an early stage.
Limited surgical resection
A limited surgical resection (also called a wedge resection) removes the section of the stomach wall that contains the tumour along with a margin of healthy tissue around the tumour. A limited surgical resection is sometimes used to treat small (smaller than 3 cm), early stage stomach cancer.
A limited surgical resection may be done by open surgery to the abdomen (called
a laparotomy) or by
Gastrectomy
A gastrectomy is the most common surgery used to treat stomach cancer. It
removes all or part of the stomach. Sometimes other organs or areas are removed
during a gastrectomy, such as the
The surgeon usually makes a large cut (incision) in the abdomen to remove the stomach. In recent years, some surgeons are doing laparoscopic surgery. For this type of surgery, the surgeon makes several small cuts and then inserts an endoscope and special tools to remove the stomach.
The type of gastrectomy done depends on the stage and where the cancer is within the stomach.
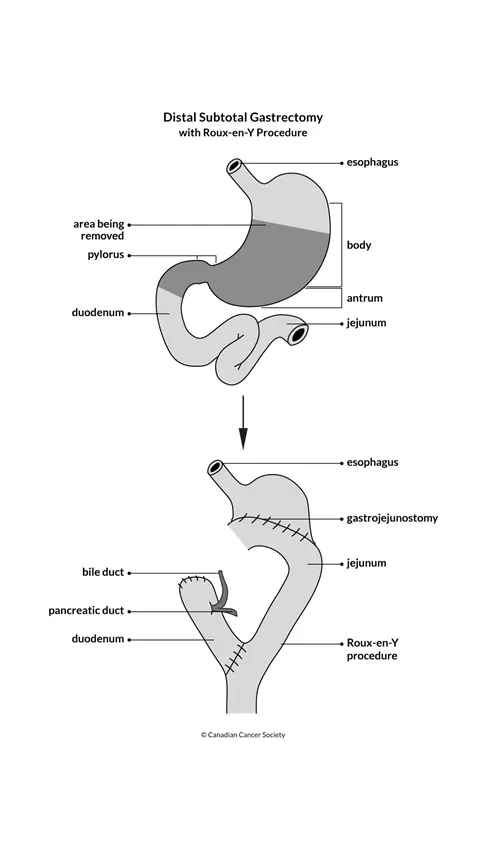
Distal subtotal gastrectomy
A distal subtotal gastrectomy is only used for tumours in the lower (distal) part of the stomach. It is not used for tumours in the fundus (top, rounded area of the stomach) or the gastroesophageal junction (where the esophagus joins the stomach).
This surgery removes:
- the lower part of the stomach, including the tumour along with an area of healthy tissue around it (called the surgical margin)
-
part of the
duodenum - nearby lymph nodes around the stomach
The GI tract is reconstructed by connecting the
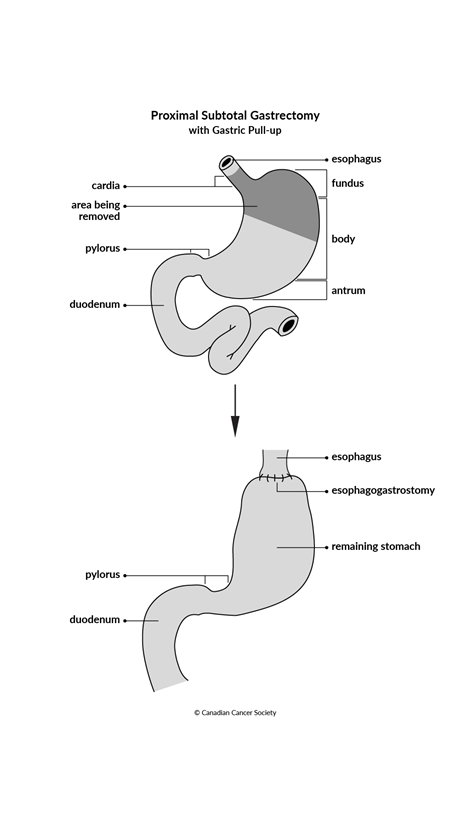
Proximal subtotal gastrectomy
A proximal subtotal gastrectomy is used for tumours in the upper (proximal) part of the stomach and in the area where the stomach joins the esophagus (called the gastroesophageal junction). This surgery removes:
- the upper part of the stomach
-
some or all of the lower part of the
esophagus - nearby lymph nodes around the stomach
The GI tract is then reconstructed by pulling up the remaining part of the stomach to the remaining upper part of the esophagus (called a gastric pull-up).
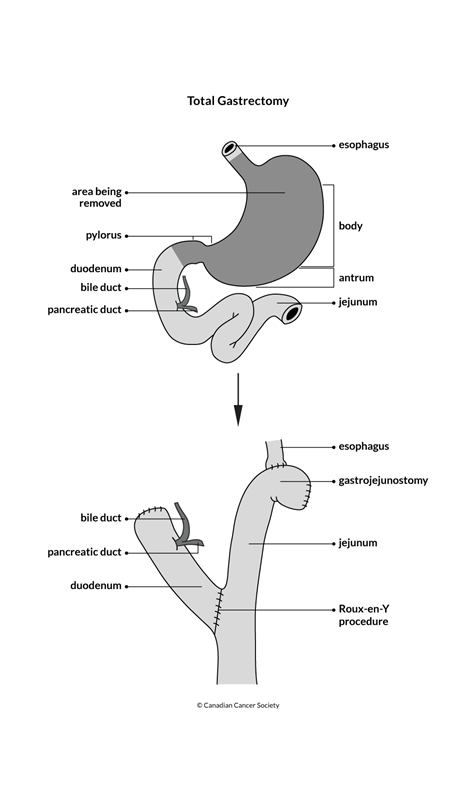
Total gastrectomy
A total gastrectomy is used for stomach cancer that has spread throughout the stomach or for a stomach tumour in the middle or upper part of the stomach. This surgery removes:
- the whole stomach
- the lower part of the esophagus
- the first part of the duodenum
- part or all of any nearby organs, such as the pancreas, spleen or liver, where the stomach tumour has spread
- nearby lymph nodes around the stomach
The GI tract is then rebuilt (reconstructed):
- The remaining part of the duodenum is separated from the jejunum, but the duodenum is still attached to the bile duct and pancreatic duct.
- The jejunum is connected to the remaining end of the esophagus.
- The remaining duodenum is connected farther down the jejunum from where the esophagus and jejunum are attached (called a Roux-en-Y procedure).
This reconstruction allows the bile and pancreatic juices to enter the digestive system without harming the remaining esophagus.
Lymph node dissection
A lymph node dissection is surgery to remove several lymph nodes from the body. It is done for stomach cancer during gastrectomy surgery.
A lymph node dissection is classified by the location of the lymph nodes that are removed. A D1 lymph node dissection removes the lymph nodes attached to the outer wall of the area of the stomach that contains the tumour. A D2 lymph node dissection removes D1 lymph nodes plus the lymph nodes around several large blood vessels near the stomach. A D2 lymph node dissection is a longer and more complicated surgery.
Find out more about a lymph node dissection.
Palliative surgery
Surgery may be used to relieve the symptoms of advanced stomach cancer including:
- bleeding
- pain
- the inability to eat
- an obstruction or a blockage (the tumour may block the passage of food into or through the stomach)
- a perforation (the tumour may grow through the wall of the stomach, creating a hole into the abdomen)
The type of palliative surgery will depend on your symptoms, the location of the stomach tumour and your overall health.
Stomach bypass surgery
Surgery may be done to change the flow of food or fluids around a tumour that is blocking the stomach or esophagus. The part of the stomach that is above the blockage is cut and then reattached to the small intestine. This allows the food to move through the stomach and into the small intestine. Stomach bypass surgery is also called a gastrojejunostomy.
Stomach bypass surgery may be done if you cannot have a gastrectomy because of health problems or if removing the tumour would not improve your quality of life.
Surgery for a bowel obstruction
A bowel obstruction is when the small intestine or colon is partly or completely blocked. The blockage prevents food, fluids and gas from passing through the intestines normally. If you have a bowel obstruction, you may need surgery to remove or bypass the part of the intestine that is blocked.
Limited surgical resection or subtotal gastrectomy
A limited surgical resection (described above) may also be used for people with advanced stomach cancer. The goal is to remove as much of the tumour as possible to try to relieve a blockage or bleeding that is hard to stop.
Placement of a stent
A stent is a hollow metal or plastic tube. Stents may be used if a tumour is blocking the opening of the stomach near the esophagus. It will allow a person with advanced stomach cancer to swallow more easily. A stent may also be placed at the opening to the duodenum to allow food to pass from the stomach into the small intestine.
The doctor places the stent using an endoscope. The endoscope is passed through the mouth, down the esophagus and into the stomach.
Feeding tube placement
If surgery or other treatments cannot relieve a blockage caused by a stomach tumour, a feeding tube may be placed through a surgical opening in the abdomen. A feeding tube may also be used for a short time after surgery for stomach cancer.
A feeding tube is used to give liquid nutrition to help maintain a healthy weight. The tube may also be used to give medicines. A feeding tube may be placed into the:
- stomach (called a gastrostomy tube, or G-tube)
- small intestine (called a jejunostomy tube, or J-tube)
Endoscopic tumour ablation
Endoscopic tumour ablation uses laser surgery to destroy some of the stomach tumour. This technique may be used in people who can't have surgery. It may be done to stop bleeding or to relieve a tumour blockage in people with advanced stomach cancer. It may also help a person to eat more easily.
Side effects of surgery for stomach cancer
Side effects can happen with any type of treatment for stomach cancer, but everyone's experience is different. Some people have many side effects. Other people have only a few side effects.
If you develop side effects, they can happen any time during, immediately after or a few days or weeks after surgery. Sometimes late side effects develop months or years after surgery. Most side effects will go away on their own or can be treated, but some may last a long time or become permanent.
Side effects of surgery will depend mainly on the type of surgery and your overall health. Surgery for stomach cancer may cause these side effects:
- pain
- bleeding
- blood clots
- infection
- dumping syndrome
- damage to nearby organs, such as the small intestine or spleen
- leaking from where the stomach or esophagus and the small intestine were joined (called an anastomotic leak)
- lack of vitamin B12 (deficiency)
Tell your healthcare team if you have these side effects or others you think might be from surgery. The sooner you tell them of any problems, the sooner they can suggest ways to help you deal with them.
Questions to ask about surgery
Find out more about surgery and side effects of surgery. To make the decisions that are right for you, ask your healthcare team questions about surgery.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
