Breast cancer in men
Breast cancer is most often diagnosed in women, but men can also develop it. All adults have breast tissue, though male breasts are less developed. Breast cancer in men may be referred to as male breast cancer.
Less than 1% of all breast cancers occur in men. Transgender, non-binary and gender-diverse people can also develop breast cancer.
Breast cancer in men is similar to the disease in women. Most breast cancers diagnosed in men are ductal carcinoma, which start in the cells lining the ducts. Find out more about the breasts and ductal carcinoma.
Symptoms
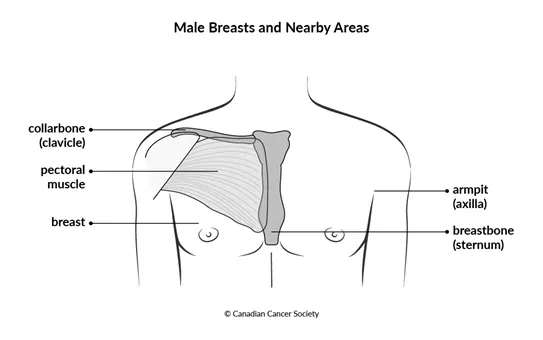
It is important to know what is normal for your breasts and the nearby areas and to report any changes to your doctor. The most common sign of breast cancer in men is a lump, often near or under the nipple.
Other signs and symptoms include:
- discharge or bleeding from the nipple
- a nipple that turns inward (inverted nipple)
- changes to the colour of the breast, such as turning red or darker than usual
- swelling or flaking of the breast
- a lump or thickening in the armpit
- an open sore (ulcer) on the skin of the breast that doesn’t heal
Find out more about the symptoms of breast cancer.
Diagnosis
Your doctor may refer you to a specialist or order tests to check for breast cancer or other health problems. Tests that are often used to diagnose breast cancer in men include mammography, ultrasound and core biopsy. Hormone receptor status testing and HER2 status testing are also an important part of diagnosis.
Find out more about diagnosis of breast cancer.
Prognosis and survival
A prognosis is the doctor's best estimate of how cancer will affect you and how it will respond to treatment. Survival is the percentage of people with a disease who are alive at some point in time after their diagnosis. Prognosis and survival for men with breast cancer depends on many factors, including the size of tumour, if there is cancer in the lymph nodes and grade.
Breast cancer in men is often diagnosed at a later stage because screening with mammography is not done like it is for women. But breast cancer survival by stage in men is similar to survival by stage in women.
Find out more about prognosis and survival for breast cancer.
Treatments
Your healthcare team will create a treatment plan just for you. The plan is based on your health and specific information about the cancer. What you want is also important when planning treatment. When deciding which treatments to offer for breast cancer, your healthcare team will consider:
- the stage of the cancer
- the grade of the cancer
- the hormone receptor status
- the HER2 receptor status
- what you prefer or want
Breast cancer in men is often treated in the same way as breast cancer in women.
A combination of treatments is usually used to treat breast cancer in men, including surgery, hormone therapy and chemotherapy.
Surgery
Surgery is a standard treatment for breast cancer in men. Depending on the stage of the cancer, you may have:
- a total mastectomy
- a modified radical mastectomy
- lymph node surgery with a sentinel lymph node biopsy or an axillary lymph node dissection
Find out more about surgery for breast cancer.
Hormone therapy
Hormone therapy adds, blocks or removes hormones to slow or stop the growth of cancer cells that need hormones to grow. Hormone therapy is usually offered to men who have breast cancer. Hormone receptor status testing is done on all breast cancers at the time of diagnosis.
Most breast cancers in men are hormone receptor–positive tumours, which means that they may respond to hormone therapy. Hormone therapy is used to lower the risk that the cancer will come back or to treat recurrent or metastatic breast cancer.
You may have one or more of the following hormone therapies.
Tamoxifen is an anti-estrogen therapy and the most common hormone therapy drug used for men with breast cancer. It is given for 5 years, and it may be offered for another 5 years if there is a high risk of the cancer coming back.
The following hormone therapies may be used to treat
- Fulvestrant may be used if the cancer keeps growing while taking tamoxifen.
- A gonadotropin-releasing hormone (GnRH) agonist drug combined with an aromatase inhibitor may be offered if tamoxifen can't be used.
- Anti-androgen drugs, such as flutamide (Euflex) or bicalutamide (Casodex) may be given to help lower the amount of androgen in the body.
- An orchiectomy is surgery to remove the testicles. The testicles make androgen, which is changed into estrogen by tissues in a man’s body. Removing the testicles lowers the amount of androgen that can be changed into estrogen, and so lowers the amount of estrogen in the body. It may be used instead of a GnRH agonist.
Find out more about hormone therapy for breast cancer.
Anti-HER2 therapy
Some drugs target specific molecules (such as proteins) on cancer cells or inside them to stop the growth and spread of cancer. Drugs that target the HER2 protein are given with chemotherapy for breast cancer in men.
The HER2 gene controls a protein on the surface of breast cells that helps them grow. Sometimes too many copies of the HER2 gene are present in a cancer cell and it makes too much HER2 protein (called HER2 positive). HER2 status testing is done on all breast cancers at the time of diagnosis.
If you have HER2-positive breast cancer, you may be given trastuzumab (Herceptin and biosimilars) in combination with chemotherapy.
Find out more about targeted therapy for breast cancer.
Chemotherapy
Chemotherapy uses drugs to destroy cancer cells. Chemotherapy is sometimes offered after surgery for breast cancer in men. You may have chemotherapy if there is a high risk that the cancer will come back.
The following chemotherapy combinations may be used to treat breast cancer in men:
- doxorubicin and cyclophosphamide followed by paclitaxel or docetaxel
- fluorouracil (also called 5-fluorouracil or 5-FU), epirubicin and cyclophosphamide followed by docetaxel
- docetaxel, cyclophosphamide
More research is needed to find out how well certain drug combinations work in men with breast cancer.
Find out more about chemotherapy for breast cancer.
Other drug therapies
Palbociclib (Ibrance) may be used to treat men with metastatic breast cancer.
Ribociclib (Kisqali) combined with fulvestrant may be used to treat
metastatic breast cancer that is hormone receptor-positive and
HER2-negative. It is used as
Zoledronic acid (Zometa) may be used if you have metastatic breast cancer that has spread to the bone. It is given to help manage and prevent problems such as hypercalcemia, bone pain and broken bones.
Find out more about targeted therapy for breast cancer and metastatic cancer.
Radiation therapy
Radiation therapy uses high-energy rays or particles to destroy cancer cells. External radiation therapy may be offered after surgery for breast cancer in men. You may be given it to the chest and nearby lymph nodes.
Find out more about radiation therapy for breast cancer.
Clinical trials
Talk to your doctor about clinical trials open to people with breast cancer in Canada. Clinical trials look at new ways to prevent, find and treat cancer. Find out more about clinical trials.
Follow-up after treatment
Follow-up after treatment is an important part of cancer care. Your healthcare team monitors your progress and recovery from treatments during regular follow-up visits. The risk that breast cancer will come back (recur) continues for 15 years or more after you are first treated.
A clinical breast exam and mammography are often done during follow-up visits.
Find out more about follow-up after treatment for breast cancer.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
