Types of breast reconstruction
If you are interested in having breast reconstruction, your plastic surgeon will discuss the different options and what may work best for you.
The types of reconstruction that may be offered after a
Breast implants
A breast implant is a round sac made of rubberized silicone. It is filled with sterile salt water (called saline) or silicone gel. Silicone implants are most commonly used in Canada.
Types of surgery for breast implants
A breast implant is placed in a space, or pocket, under or over the chest muscle. Surgeons can use the following techniques to create the pocket.
Tissue expansion
If the skin and tissues in the chest are too tight or flat for the
surgeon to place the implant under the skin or muscle, they will need to
make the space larger. This is called
An expander implant is used to create the pocket. It is an empty bag with a small valve, like a balloon. The surgeon places the expander implant under the skin or muscle on the chest. Sometimes the expander implant is placed during a mastectomy. It can also be placed during a separate surgery at a later time.
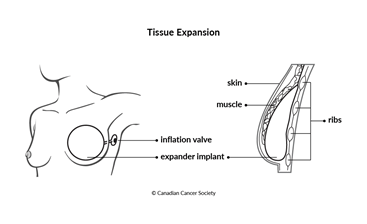
Once the expander implant is in place, the surgeon or a nurse slowly fills it with saline over a period of time. They will place a very small needle through the skin and into the valve to inject the saline. This is done in several visits to the surgeon’s office until the skin is stretched enough to fit a breast implant that is the same size as the other breast. Visits are often weekly, but this will depend on the size of the expander and what you and the surgeon feel is best.
Once the skin is stretched enough, the surgeon does a second operation to remove the expander implant and place the permanent implant. This second operation is usually done several months later.
Direct-to-implant reconstruction
Direct-to-implant reconstruction is done less often than tissue expansion. It may be an option if you don't have enough tissue available on your body that can be used to make a breast.
Direct-to-implant reconstruction may also be called a single-stage breast reconstruction. This is because it can be done in a single surgery. Instead of first using an expander implant, the surgeon will place the breast implant during a mastectomy or breast-conserving surgery.
For direct-to-implant reconstruction, the surgeon commonly uses
acellular dermal matrix (ADM). ADM is a
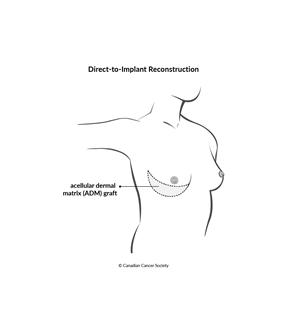
The surgeon will stitch the ADM product to the chest to create a pocket for the breast implant, which is then placed under or over the muscle. ADM may also be used to cover the edges of an implant.
The ADM acts as a supportive scaffold, like a sling. It helps keep the implant in position. Your own blood vessels grow into the ADM so that over a few months, your body naturally incorporates the ADM.
Direct-to-implant reconstruction using ADM may not be available everywhere in Canada. If you are interested in implant reconstruction, talk to your plastic surgeon to find out if this type of reconstruction is an option for you.
Removing breast implants
A breast implant is not permanent. You can have it removed if you decide that you don’t want to have it any more.
Breast implants may last 10 to 15 years before they need to be removed or replaced. As an implant gets older, the risk of rupture increases. A rupture is when the silicone or saline leaks out of a hole in the implant.
You may also need to have an implant removed or replaced if it moves or changes shape or if too much scar tissue forms around it.
After a breast implant is removed, you may have dimpling, puckering, wrinkling or other changes to how your skin looks in the area where the implant was.
Side effects and complications
Different types of surgery can cause different
Side effects and complications of breast implant surgery will depend mainly on the type of surgery and your overall health. If you had radiation therapy to the chest as part of breast cancer treatment, your surgeon may not recommend breast implants because you may have more complications after surgery.
Tell your healthcare team if you have side effects and complications that you think are from your implant surgery. The sooner you tell them of any problems, the sooner they can suggest ways to help you deal with them.
Possible side effects and complications from breast implant surgery include:
- infection
-
buildup of fluid (called
seroma ) in the breast - pain
-
scar tissue around the breast implant (called
capsular contracture ) , which makes the breast feel hard and lose its shape - movement of the implant
- wrinkling of the implant, which makes the skin on the breast wrinkle (called animation)
- leaking or breaking of the implant
You may have concerns about how breast implants could affect your health. In very rare cases, women with silicone gel or saline breast implants can develop a type of non-Hodgkin lymphoma (NHL) called breast implant–associated anaplastic large-cell lymphoma (BIA-ALCL). It starts in the scar tissue that forms around the implant.
Health agencies around the world are still collecting information about how many women are diagnosed with BIA-ALCL. Research suggests that the risk for BIA-ALCL is only related to textured implants rather than those with smooth surfaces. In 2019, Health Canada suspended the medical license for the one brand of textured breast implants that were available in Canada.
Autologous breast reconstruction
Autologous breast reconstruction uses skin, fat and sometimes muscle from other parts of your body to create a new breast. The reconstructed breast has a more natural feel than a breast implant.
Tissue techniques
To do an autologous breast reconstruction, the surgeon creates a "flap" from tissues in your body. This flap is usually taken from your abdomen, but it can also be taken from your back, buttock or thigh. It includes blood vessels, skin, fat and sometimes muscle. The surgeon will use the flap to rebuild the breast.
A free flap is a common technique used for autologous breast reconstruction. It is called a free flap because the surgeon completely removes the flap from its blood supply. The surgeon then places the flap on the chest and attaches it to the blood supply there.
A pedicle flap keeps the tissue attached to its original blood supply. The surgeon tunnels the flap under the skin to the chest to rebuild the breast.
Types of flaps used for breast reconstruction
There are several types of flaps used to reconstruct a breast. Your plastic surgeon will discuss the options and help you decide what is best for you.
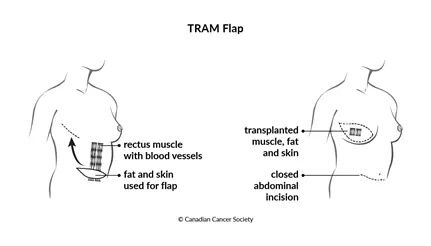
A
pedicled transverse rectus abdominus muscle (TRAM) flap
uses muscle, fat, skin and blood vessels from your abdomen to reconstruct
your breast. The area on your abdomen is repaired with a special mesh to
restore the strength of the
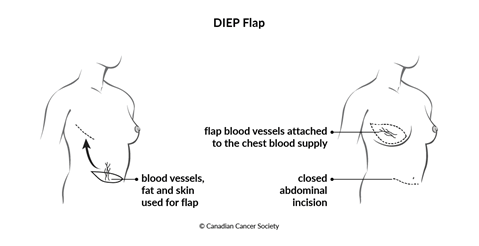
A deep inferior epigastric perforator (DIEP) flap uses only fat, skin and blood vessels from your abdomen. Unlike the TRAM flap, it doesn't take muscle from your abdomen.
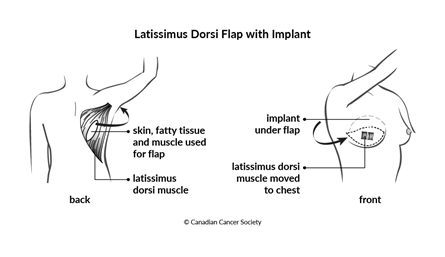
A latissimus dorsi (LD) flap is also called a back flap. It uses the muscle called the latissimus dorsi, or "lat," fat and skin from your back to make a mound to rebuild the breast. A breast implant can be used if there isn’t enough tissue to make a natural-looking breast. This type of flap is used if you had radiation therapy to your chest or if you don’t have any extra skin and tissue on other areas of your body that can be used for breast reconstruction.
Other free flaps use skin, fat and blood vessels from other areas of your body to reconstruct your breast. Tissue may be taken from your lower back, buttocks or your upper thighs. These types of free flaps are less common than ones that use tissue from your abdomen.
Side effects and complications
Side effects and complications of autologous breast reconstruction will depend mainly on the type of surgery, where the flap tissue comes from and your overall health. If you have larger breasts or had radiation therapy to the chest, you may have more complications after autologous breast reconstruction.
Tell your healthcare team if you have side effects or complications you think might be from your breast reconstruction surgery. The sooner you tell them of any problems, the sooner they can suggest ways to help you deal with them.
Autologous breast reconstruction may cause:
- infection
- bleeding
-
fluid buildup (
seroma) where the tissue was taken from - scars where the tissue was taken from
- breasts that aren’t the same size or shape
- weakness and bulging of the abdominal muscles in the area where the muscle was removed (hernia)
- slightly different colour and texture of the reconstructed breast compared to the rest of the breast area
- less muscle strength in the back if tissue to rebuild breast was taken from there
If you smoke, it's strongly recommended that you quit at least 3 months before having an autologous breast reconstruction. Smoking affects blood flow to the skin and underlying tissues, which can lead to infection, delayed healing and a higher risk that the tissue in the flap will die (called flap necrosis).
Nipple and areola reconstruction
The nipple and areola (the dark-coloured skin around the nipple) may need to be removed during a mastectomy. If the nipple and areola were removed, the surgeon can rebuild them to create a more natural-looking breast.
Nipple and areola reconstruction is the final step of breast reconstruction and can be done as an outpatient surgery. This procedure is done after the reconstructed breast has fully healed, which is at least 3 to 6 months after breast reconstruction surgery.
The tissue used for nipple reconstruction comes from the newly created breast. The surgeon can also use skin from other parts of the body such as the chest or earlobes.
The reconstructed nipple and areola may be a slightly different colour than the other breast. If this happens, a medical tattoo artist can tattoo the areola to better match the colour of your opposite breast. This may be done a few months after nipple and areola reconstruction. The artist uses a 3D tattoo technique, which uses colour and shading to make it resemble a natural nipple as much as possible.
A reconstructed nipple has much less feeling than a natural one. For this reason, you may also choose to just get the tattoo and not do nipple and reconstruction surgery.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
